How do we take care of the caretakers who are saving our lives?
How do we take care of the caretakers who are saving our lives?
-by Vince Bzdek
(Originally published in “The Gazette”)
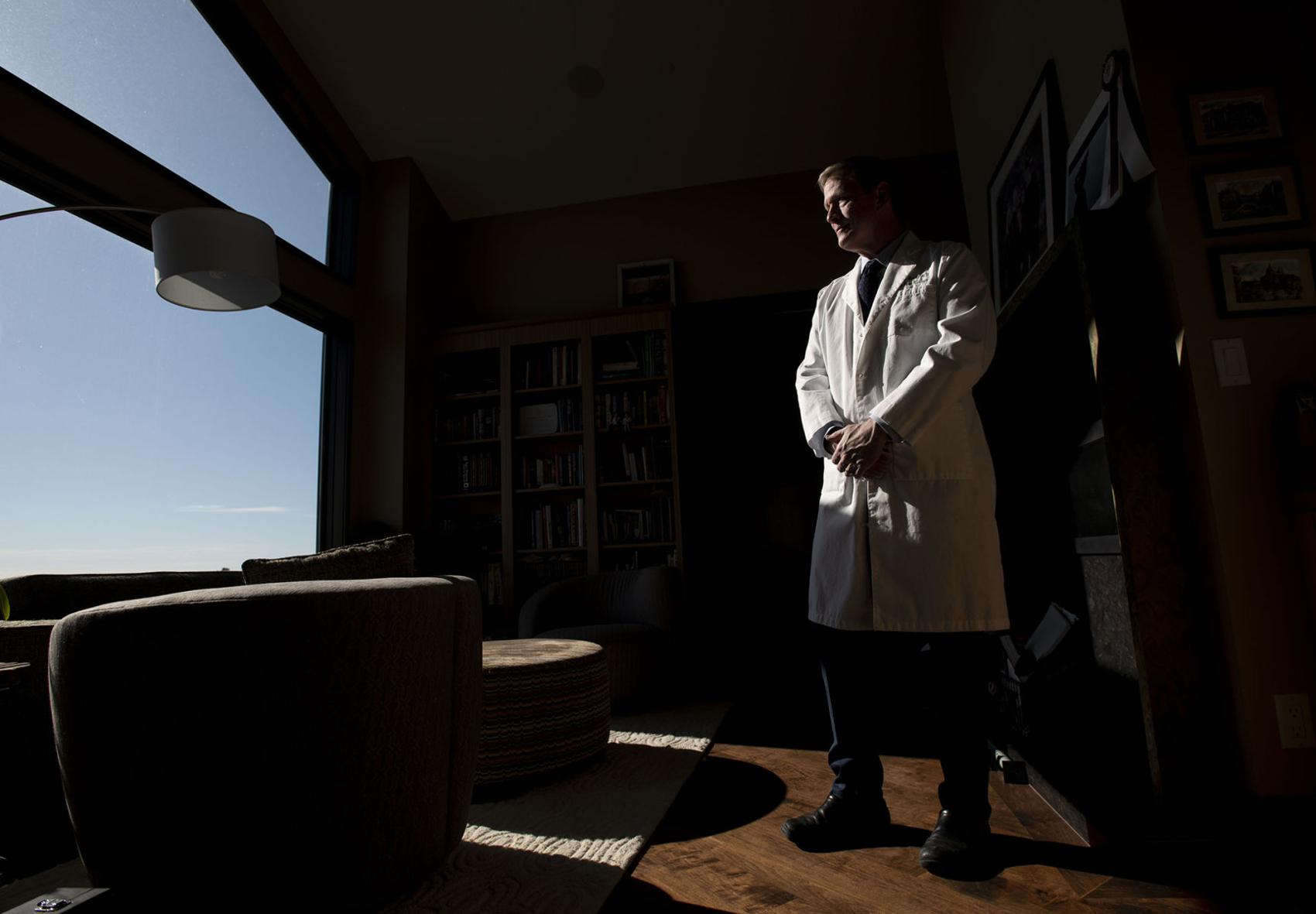
Dr. Jeff Moody, a urologist, at his home in Colorado Springs in April. Studies show burnout is very high for physicians, said Moody, “and it’s up another 20% to 30% since March” because of COVID. Moody wrote a book, “The Doctor is Burned Out.”
Who do you know on the front lines of the battle against COVID-19?
We all know someone. A pulmonologist who is in the ICU all day every day caring for patients at Memorial Hospital. Urgent care nurses shuttling from hospital to hospital, and even state to state, to help where the need is most acute. The masked men and women administer hundreds of daily tests to the potentially infectious at the drive-thru testing center in the parking lot at The Citadel mall.
I talked to a physician friend, Jeff Moody, this week after he’d gotten three hours sleep because he was on call the night before at Memorial and St. Francis hospitals and had to take a couple cases during the middle of the night.
Moody said it’s the nurses he admires the most. He recently had to operate on a patient who was showing COVID symptoms and said he was unbelievably impressed with the nursing care and their dedication. “They were like 24/7, 12-hour shifts, all day soaking in the risk of COVID caring for these people,” Moody said. “To me the doctors are obviously on the front lines, but I think the nursing personnel are the real heroes of all this because they’re providing all the direct care. The exposure is unbelievable. They don’t eat so they don’t have to take off their masks.”
It’s been eight grueling months for our health care workers, and I worry greatly about the toll COVID is taking. Local hospitals tell us they are more worried about staff shortages than capacity issues right now.
Who’s taking care of our caretakers?
“Today, we got an email from one of the hospitals systems asking if we wanted to volunteer time working with COVID patients. A plea for any physicians of any kind to volunteer,” Moody said, even if they had no particular expertise in treating COVID patients, which shows how desperate hospitals are for health care workers.
Studies show burnout is already very high for physicians, said Moody, “and it’s up another 20% to 30% since March” because of COVID.
Moody wrote a book, “The Doctor is Burned Out,” just before COVID hit, but his observations and recommendations couldn’t be more relevant and timely now for health care workers who have been risking their lives for the rest of us.
“More than 50% of physicians are clinically burned out, 70% would not recommend medicine as a career, one in seven is suicidal and one per day completes suicide,” Moody writes. “I want this book to take the dark curtain off physicians in need of help and let them step into the light of healing.”
Moody’s book is a humane, practical prescription for what health care workers can do about burnout and stress, and what the industry needs to do, but his is a personal story of burnout and coping with burnout as well, which is what makes Moody’s story resonate. And matter. His book reminds us that the people saving us are real, vulnerable people, showing us how human they all are.
“Shining the light on myself, I hope, will encourage others to recognize their own issues, seek care, and no longer feel the stigma of seeking care for mental health issues,” Moody wrote.
Moody talked to me frankly this week about what burnout looks like.
His definition in his book captures exactly what health care workers have likely endured for the last eight months: “A state of emotional and physical exhaustion caused by a prolonged period of stress and frustration; an inevitable corporate condition characterized by frequent displays of unprofessional behavior, a blithe refusal to do any work, and most important, a distinct aura of not giving a s—.”
Moody, a UCLA-trained urologist, has lived through diagnosis, treatment and recovery from clinical burnout himself. He sponsors a monthly Physician Burnout Support Group in town.
Moody told me he had moments of suicidal ideation before treating his own burnout.
“The first time I ever admitted that to myself was while writing this book,” he said.
He’s not alone. Physicians have the highest rate of suicide as a profession. While he was writing the book, one of his favorite doctors committed suicide.
“It is estimated that an entire medical school commits suicide every year, or about 400 doctors. That’s more than one every day,” Moody said.
“What happens to all the families of those physicians who are gone? It’s like a never-ending, expanding circle of effect. The average doctor sees about 2,500 patients a year. That’s a million patients a year impacted.”
And the current circumstances for doctors are making things worse.
“Burnout burns much more brightly in isolation,” Moody said.
The best thing that is happening right now, Moody says, “is that we’re starting to allow the conversation to occur about being a real person, and having problems, and having mental health issues.”“I gave a talk recently on mental health in the time of COVID, and I told the workers, you have to control the things you can control, and know what those are. Other than that you have to allow yourself to not perseverate on the things you can’t control, like will I get it or not, or will I get really sick if I get it or not. But you can do everything possible to protect yourself and protect your family.”
As he was writing the book, Moody was counseled that changing individual behaviors is one thing, changing the corporate health care system itself is nearly impossible.
“Medicine in general has evolved into this 1950s manufacturing production model where it’s like you’re a widget in an assembly line and if you break down they’ll just throw you out and get somebody else because all doctors are exactly the same,” Moody observes.
“What is the health care system designed to do?” Moody asks. “Well, it’s supposed to care for people. Damnit, let’s put the caring back into the system,” not just for patients, but for practitioners as well.
You can’t have a sick system caring for the sick.
Moody believes the current system with its growing, endless demands and more finite resources is unsustainable, and it needs to reinvent itself as a physician-wellness focused system.
Some hospital systems have told their front line workers that they would guarantee them three months employment during this crisis and that’s it. That kind of uncertainty sure makes it hard on our front-line workers to do their jobs effectively.
“The brain chemistry is much better when you’re in a problem-solving mode than when you’re in a reactive or fear mode,” adds Moody. “That’s the kind of the footing I like to get people on. Let’s talk about solving problems, then we’re working together toward something instead of sitting around complaining and moaning about poor us, and we’re going to be bankrupt in six months. Let’s take the lemons and make frickin’ lemon soufflé.
Moody tells the story of a family practitioner who was out of work during the April shutdown. “What can we do?” she asked a lawyer friend. “She couldn’t work because their clinic was closed, so they said let’s do something.”
They were worried at the time about the personal protective equipment ( PPE) shortage for health care workers. “And they’re like, well we have all these shipping containers, and in a matter of over a month they developed this company where they take shipping containers, put N95 masks in and sterilize them very quickly and they could run like hundreds of thousands of batches of masks a day.
“The ingenuity of the American people is pretty amazing. I think that’s maybe our No. 1 advantage in the world.”
Changing the system starts with engaging the system, Moody says.
“The best thing you can do is really maintain open communication with your hospital,” Moody tells health care workers. “I’m kind of a believer that if you give first, people will give back to you. I would go to the hospital and say how can we help, what ideas do I have, and what are ways that we can work together? Then, once they are kind of in your debt, then you can say, here’s how you can help me.”
Check out my video of the week:
If I could do only one exercise, it would be yoga. It is cardio, resistance training, stretching, and relaxation all at the same time. I think it keeps the muscles and joints from ossifying further, and it is good for the mind. By using the techniques I share about in today’s video, it will allow you to refocus on what is important and have some perspective on the events of the day.
→If you’re looking for burnout answers, grab a copy of my new Book:
→Check out my NEW live stream series, Burnout Breakthrough on @JeffMoodyMD.
What did you think of this video training?
+ Leave a comment below and let me know what you struggle with and which tip made a difference for you.
+ Share this video with others so they can get the inside scoop.
Have a topic you’d like me to share tips about? I’d love to hear from you!
Jeff Moody, MD, Author
The Doctor is Burned Out: A Physician’s Guide to Recovery
Lioncrest Publishing, 2020
// OTHER PLACES TO FIND ME //
Share this post!
You Are Not Alone
Sign Up for our Newsletter for more information!
I help you get these results with a systematic approach to diagnosing, treating and recovering you from burnout.